Background: CPX-351, a liposomal formulation of daunorubicin and cytarabine in the fixed molar ratio (1:5), is approved for the treatment of adult patients (pts) with newly diagnosed acute myeloid leukemia (AML) with myelodysplasia-related changes and therapy-related AML (t-AML). To explore the potential benefit of CPX-351 in a broader indication, we initiated a randomized phase III study of CPX-351 vs "3+7" in pts ≥18 years (yrs) of age with AML and intermediate or adverse genetics according to 2017 European LeukemiaNet (ELN) risk categorization (AMLSG 30-18, NCT03897127). In the younger pts (18-60 yrs) we sought to investigate a higher dose of CPX-351. We here report data from an interim safety analysis for this higher CPX-351 dose.
Methods: Pts are randomized to receive first induction cycle (ind 1) with either CPX-351 or daunorubicin + cytarabine ("3+7": daunorubicin 60 mg/m2 on days 1, 2, 3 + cytarabine 200 mg/m2 on days 1-7); in pts aged 18-60 yrs (performance status 0-1) CPX-351 is given at a dose of 55 mg/m2 daunorubicin/125 mg/m2 cytarabine (125 U/m²; 1 U/m2=0.44 mg/m2 daunorubicin/1 mg/m2 cytarabine; days 1, 3, 5); pts >60 yrs receive the standard dose CPX-351 100 U/m² (days 1, 3, 5). There was no age-adapted dosing in the control arm. For induction cycle 2 (ind 2), pts on the CPX-351 arm receive the same dosage on day 1+2 only; pts on the control arm receive intermediate-dose cytarabine + daunorubicin (both in age-adapted dosing). Continuous assessment for safety is performed for two endpoints: 60-day mortality with a maximally tolerated rate (MTR) of 15%; and hematologic recovery times with i) neutropenia 4° and / or ii) thrombocytopenia 3° or 4° after each ind lasting longer than day 42 after start of treatment cycle (without evidence of persistent leukemia) with a MTR of 25%. Median hematologic recovery times were analyzed using Kaplan-Meier estimates, p-values are mentioned in a descriptive manner (log-rank test).
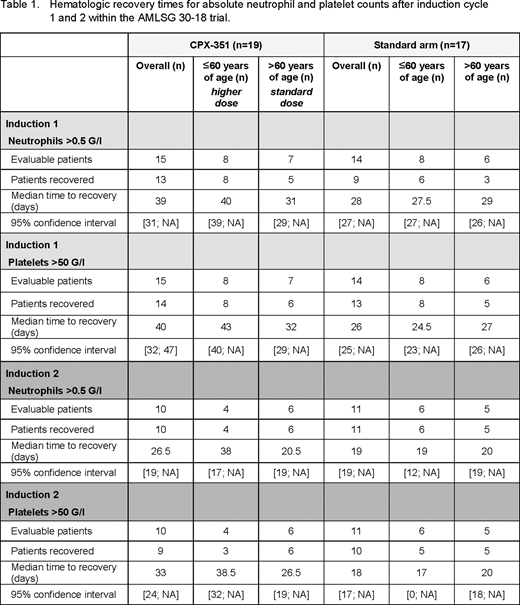
Results: As of July 20, 2020, 36 patients have been randomized to the study (CPX-351, n=19; "3+7", n=17) with following characteristics: de novo AML, n=27, secondary or t-AML, n=9; median age 60.5 yrs (range 47-75; ≤60 yrs, n=18; >60 yrs, n=18); intermediate and adverse risk genetics were found in 7 and 10 pts, respectively (not available yet, n=19). On the CPX-351 arm, 9 of 19 pts were ≤60 yrs of age and received the higher CPX-351 dose. So far, 36 pts received ind 1, 25 pts ind 2. Overall, the median time to neutrophil recovery with absolute neutrophil count (ANC) >0.5 G/l was longer in the CPX-351 arm compared to the "3+7" arm: 39 vs 28 days (p=0.07) after ind 1, and 26.5 vs 19 days after ind 2 (p=0.06; table 1). Time to platelet recovery >50 G/l was significantly prolonged in the CPX-351 arm after ind 1 (40 vs 26 days; p<0.0001), currently not after ind 2 (33 and 18 days; p=0.35). When comparing the higher dose (125 U/m²; pts 18-60 yrs) with the standard CPX-351 dose (100 U/m², pts >60 yrs), the median time to neutrophil recovery after ind 1 was significantly longer with the higher dose (40 and 31 days, respectively; p=0.03); after ind 2 median times were 38 and 20.5 days (p=0.26); platelet recovery (>50 G/l) was also significantly delayed after ind 1 with the higher compared to the standard CPX-351 dose (median 43 vs 32 days; p=0.002); platelet recovery after ind 2 was after a median of 38.5 and 26.5 days, respectively (p=0.17). There was no treatment-related death (60-day mortality 0%) in both arms. So far, 6 of the 9 pts (67%) treated with the higher CPX-351 dose reached the safety endpoint of persisting neutropenia (n=4) or thrombocytopenia (n=5) during ind beyond day 42. The MTR was exceeded for thrombocytopenia (0.63; 95% confidence interval (CI) [0.31; 0.86]), but not for neutropenia (0.50; 95% CI [0.22; 0.78]). Overall, there were 18 serious adverse events (SAEs); among the most frequent SAEs were infections and fever in neutropenia (n=10).
Conclusion: The higher dose of CPX-351 administered in pts 18-60 yrs of age led to significantly prolonged hematologic recovery times during ind 1 and 2 exceeding the MTR for thrombocytopenia without treatment-related death. Based on the prolonged hematologic recovery, the protocol will be amended, in that the CPX-351 dose for ind in pts 18-60 yrs of age is reduced to the current Package Insert for CPX-351 44 mg/m2 daunorubicin / 100 mg/m2 cytarabine (100 U/m²). Data on hematologic response as well as on measurable residual disease using multi-parameter flow cytometry will be presented.
Kapp-Schwoerer:Jazz Pharmaceuticals: Honoraria, Research Funding. Thol:Daiichi Sankyo: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees; Astellas: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees. Heuser:Karyopharm: Research Funding; Abbvie: Consultancy; Astellas: Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Roche: Research Funding; BerGenBio ASA: Research Funding; Janssen: Consultancy; Stemline Therapeutics: Consultancy; Bayer: Consultancy, Research Funding; Daiichi Sankyo: Consultancy, Research Funding; Amgen: Research Funding; PriME Oncology: Honoraria. Faderl:Jazz Pharmaceuticals: Current Employment, Current equity holder in publicly-traded company. Wagner:JAZZ Pharmaceuticals: Current Employment; JAZZ Pharmaceuticals: Current equity holder in publicly-traded company. Ganser:Celgene: Consultancy; Novartis: Consultancy. Döhner:Abbvie: Consultancy; Daiichi Sankyo: Honoraria; Celgene: Consultancy, Honoraria; Jazz Pharmaceuticals: Consultancy, Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Astex Pharmaceuticals: Consultancy; Roche: Consultancy; Bristol-Myers Squibb: Research Funding; Pfizer: Research Funding; Amgen: Consultancy, Research Funding; Astellas Pharma: Consultancy; Janssen: Consultancy, Honoraria; Sunesis Pharmaceuticals: Research Funding; Agios: Consultancy; Arog: Research Funding. Paschka:BerGenBio ASA: Research Funding; Janssen Oncology: Other; Amgen: Other; Otsuka: Consultancy; Novartis: Consultancy, Speakers Bureau; Sunesis Pharmaceuticals: Consultancy; Pfizer: Consultancy, Speakers Bureau; Astellas Pharma: Consultancy, Speakers Bureau; Celgene: Consultancy, Other: Travel, accommodations or expenses; Jazz Pharmaceuticals: Consultancy, Speakers Bureau; Agios Pharmaceuticals: Consultancy, Speakers Bureau; Astex Pharmaceuticals: Consultancy; AbbVie: Other: Travel, accommodation or expenses, Speakers Bureau. Döhner:Abbvie: Consultancy, Honoraria; Sunesis: Research Funding; Roche: Consultancy, Honoraria; Pfizer: Research Funding; Oxford Biomedicals: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Helsinn: Consultancy, Honoraria; Jazz: Consultancy, Honoraria, Research Funding; AstraZeneca: Consultancy, Honoraria; AROG: Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Agios: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Astellas: Consultancy, Honoraria, Research Funding; Astex: Consultancy, Honoraria; GEMoaB: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Bristol Myers Squibb: Consultancy, Honoraria, Research Funding.
CPX-351 is approved for the treatment of adult patients with newly diagnosed acute myeloid leukemia (AML) with myelodysplasia-related changes and therapy-related AML (t-AML). To explore the potential benefit of CPX-351 in a broader indication, a randomized phase III study of CPX-351 vs 3+7 in patients older than 18 years of age with AML and intermediate or adverse genetics according to 2017 European LeukemiaNet (ELN) risk categorization (AMLSG 30-18, NCT03897127) was initiated. In the younger patients (18-60 yrs) a higher dose of CPX-351 is evaluated.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal